World’s First AI Clinic Launches in Saudi Arabia to Treat 50 Diseases
On May 16, 2025, Saudi Arabia opened the world’s first AI-operated doctor clinic—Dr. Hua—initially covering 30 respiratory conditions and expanding to 50 diseases, combining AI diagnosis with human approval.
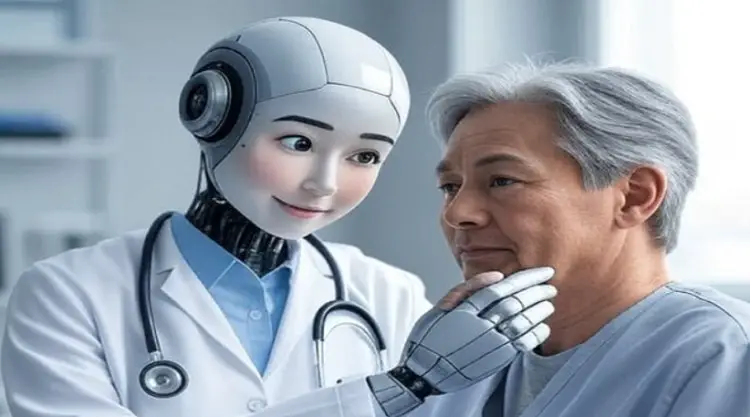
The integration of artificial intelligence (AI) into healthcare is transforming how medical services are delivered around the globe. From telemedicine consultations to AI-driven diagnostic tools, technology is reshaping the patient experience. Yet on May 16, 2025, Saudi Arabia took a historic step by inaugurating the world’s first fully AI-operated doctor clinic in Al-Ahsa. A collaboration between Shanghai’s Synyi AI and the local Almoosa Health Group, this clinic—powered by an AI physician named “Dr. Hua”—aims to diagnose and treat fifty different conditions, beginning with thirty respiratory ailments and expanding to cover a broad range of diseases within the next year.
This article explores the motivation behind the project, how Dr. Hua works, which diseases are included, the benefits and challenges of the model, its global implications, and recommendations for policymakers and patients alike.
1. The Need for AI-Driven Healthcare
1. Shortage of Medical Professionals
Many regions—especially rural or underserved areas—struggle with a scarcity of qualified doctors and specialists. Patients often travel long distances and face long waiting times for consultations, putting strain on both families and healthcare systems.
2. Rise of Telemedicine
The COVID-19 pandemic accelerated telemedicine adoption, allowing doctors to consult patients remotely. However, even telehealth remains dependent on human practitioners whose availability can be limited.
3. Digital Transformation in Saudi Arabia
As part of its Vision 2030 plan, Saudi Arabia has prioritized digital innovation across sectors, including healthcare. The launch of the AI clinic in Al-Ahsa addresses both access and quality of care by deploying an autonomous diagnostic system complemented by human oversight.
2. Meet Dr. Hua: The AI Doctor
At the heart of the clinic is Dr. Hua, an advanced AI model trained on millions of anonymized patient records, imaging studies, and clinical guidelines. Here’s how a typical patient encounter unfolds:
1. Registration & Symptom Entry
Upon arrival, patients use a touchscreen tablet to enter basic demographics—name, age, gender, height, weight—and describe their symptoms through structured questionnaires.
2. Interactive AI Interview
Dr. Hua conducts a guided interview, asking follow-up questions such as “When did your symptoms start?”, “Have you experienced any fever?”, or “Are you currently on any medications?” This dynamic questioning adapts based on the patient’s responses.
3. Multimodal Data Analysis
Patients can upload lab results, imaging scans (X-rays, ultrasounds), and ECG tracings. Dr. Hua’s deep-learning algorithms analyze both structured data (e.g., blood counts) and unstructured data (e.g., radiology images) to identify patterns.
4. Preliminary Diagnosis & Probability Scoring
The AI generates a ranked list of possible diagnoses, each accompanied by a probability score. For instance, it might suggest:
o Bronchitis (68% probability)
o Early-stage pneumonia (24%)
o Viral pharyngitis (8%)
5. Treatment Plan & Lifestyle Recommendations
Dr. Hua drafts a treatment regimen—medication dosages, breathing exercises, dietary advice, and follow-up tests. For example, an asthma patient might receive inhaler instructions plus lifestyle modifications.
6. Human Doctor Approval
A licensed physician reviews the AI’s findings and plan, making any necessary adjustments before finalizing the consultation. This hybrid model ensures safety and builds patient trust.
3. From 30 to 50 Diseases: Scope of Care
Initial Focus: 30 Respiratory Conditions
The pilot phase covers thirty common respiratory ailments, such as:
- Asthma
- Bronchitis
- Pneumonia
- Chronic obstructive pulmonary disease (COPD)
- Pharyngitis and laryngitis
- Pulmonary fibrosis indicators
Planned Expansion to 50 Conditions
Within twelve months, the clinic will extend its services to include:
1. Gastrointestinal Disorders
o Gastritis
o Acid reflux (GERD)
o Enteritis (intestinal inflammation)
2. Dermatological Diseases
o Eczema
o Psoriasis
o Fungal skin infections
3. Musculoskeletal Issues
o Arthritis
o Carpal tunnel syndrome
4. Neurological & Other External Conditions
o Tension headaches
o Herpes zoster (shingles)
This broad portfolio will allow rural and urban patients alike to access expert-level care for a diverse set of health problems.
4. Key Benefits for Patients and Providers
1. Rapid Diagnosis
Traditional clinics can require hours of waiting. The AI model reduces initial consultation time to about 10–15 minutes, enabling patients to receive prompt care.
2. Reduced Costs
Automated processing cuts down on labor and operational expenses, translating to more affordable services for patients and lower overheads for health systems.
3. Extended Accessibility
Through telemedicine support, patients in remote areas can follow up virtually without traveling, alleviating geographic barriers.
4. 24/7 Availability
Unlike human doctors, an AI physician can provide round-the-clock consultations and preliminary evaluations, making urgent advice possible at any hour.
5. Continuous Learning
As Dr. Hua encounters more cases, its algorithms update regularly, improving diagnostic accuracy and expanding its knowledge base.
5. Challenges and Considerations
1. Data Privacy and Security
Storing sensitive health records and imaging data in encrypted cloud environments is essential to protect patient confidentiality.
2. Liability Frameworks
Clear regulations are needed to determine responsibility if an AI’s diagnosis proves incorrect: Is it the software developer, the clinic operator, or the supervising physician?
3. Building Patient Trust
Some patients may hesitate to accept AI-generated recommendations. The mandatory human-review step helps bridge this trust gap.
4. Infrastructure Requirements
Reliable internet connectivity and uninterrupted power supply are prerequisites, especially in rural settings where such resources can be scarce.
5. Algorithmic Bias
Ensuring the AI model is trained on diverse population data is critical to prevent disparities in care quality across different demographic groups.
6. Global Impact and Future Prospects
1. International Roll-out
If successful, this hybrid AI-clinic model could expand into Southeast Asia, Africa, and Latin America—regions facing doctor shortages and logistical hurdles.
2. Enhanced Remote Healthcare
Future integrations may include at-home testing kits, AI-driven wearable monitoring, and virtual reality–assisted rehabilitation for chronic conditions.
3. Medical Research Advancements
Aggregated, anonymized data from thousands of patient encounters can accelerate drug discovery, epidemiological studies, and personalized medicine initiatives.
4. Cost Reduction Across Systems
Health insurers and government payers may see decreased expenditure by shifting routine diagnostics from high-cost hospital settings to AI-powered clinics.
5. Next-Gen Technologies
Upcoming additions might feature robotic surgery assistance, augmented reality (AR) for procedural training, and genomic data interpretation by AI.
7. Recommendations for Government and Citizens
1. Regulatory Frameworks
Develop national and international guidelines to govern AI in healthcare, addressing safety, ethics, and liability.
2. Data Protection Standards
Adopt stringent data-privacy laws—akin to GDPR—to safeguard patient information and enforce secure data handling.
3. Public Awareness Campaigns
Educate communities on the advantages and limitations of AI-based healthcare to foster informed acceptance.
4. Infrastructure Investments
Enhance broadband and power infrastructure in remote areas to support consistent service delivery.
5. Training Programs
Equip medical staff with skills to oversee AI tools, interpret outputs, and maintain human-in-the-loop oversight.
Saudi Arabia’s pioneering AI clinic in Al-Ahsa—powered by Dr. Hua—marks a watershed moment in global healthcare. By combining automated diagnostics for up to fifty diseases with human physician approval, the clinic delivers fast, affordable, and scalable care. As the model proves its efficacy and expands, it holds the promise of bridging healthcare gaps in underserved regions worldwide, reducing costs, and driving medical innovation. Patients can look forward to a future where expert-level diagnoses are available at the tap of a screen, and physicians can focus their skills on complex cases that truly require human judgment.
Disclaimer:
This article is based on publicly available industry reports and news releases. It is intended solely for informational purposes. Always consult qualified healthcare professionals or appropriate authorities before making medical, legal, or financial decisions.